For such a common disease, lung cancer can be hard to spot.
In the early stages you probably won’t even know you’ve got a problem. But by the time you investigate that persistent cough, your livelihood may already hinge on a range of expensive, invasive treatments.
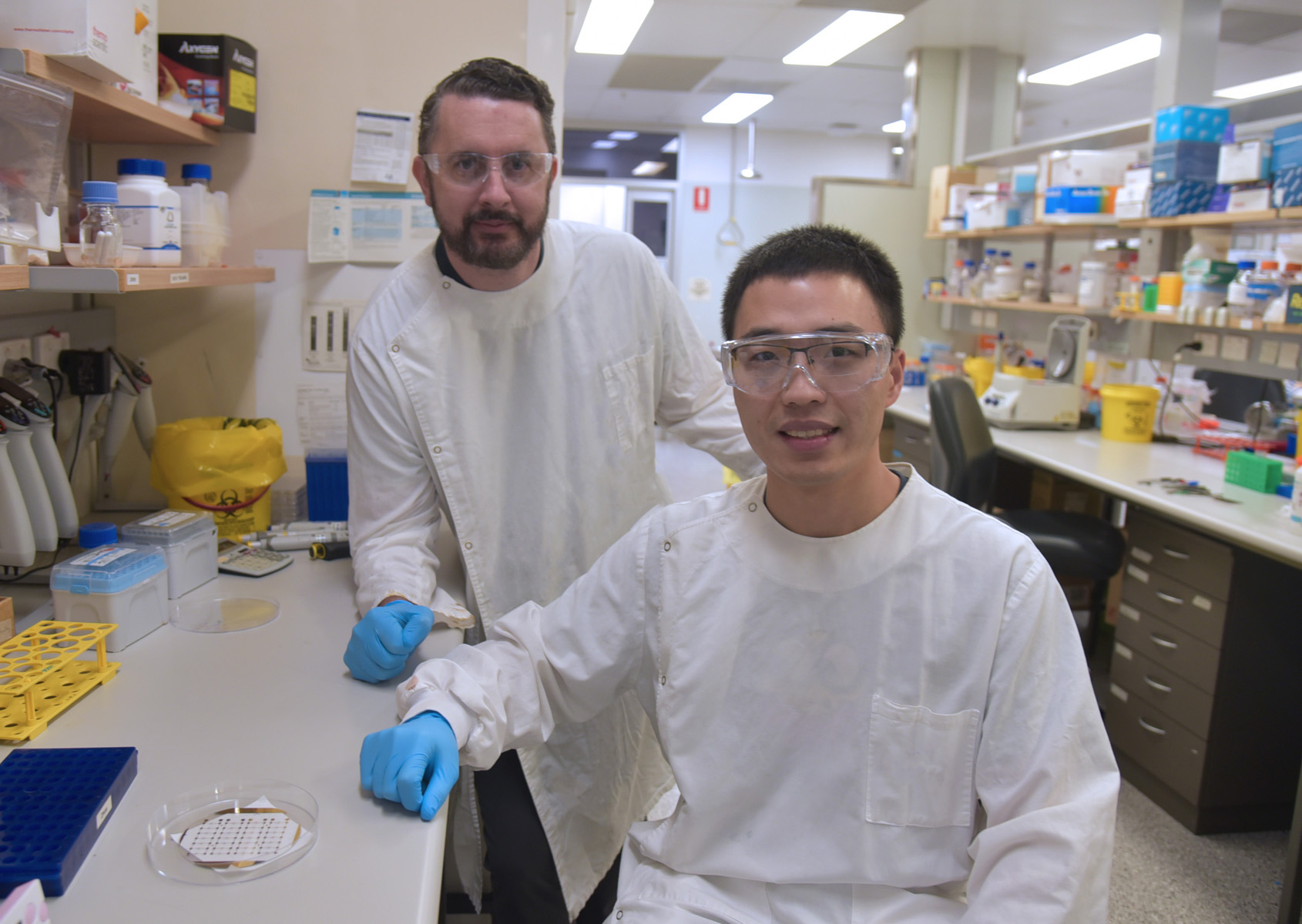
Quan Zhou and Dr Richard Lobb say it doesn’t have to be this way - and they’ve got a sugar-sensing piece of technology that proves it.
In the journal Advanced Science, researchers at the Australian Institute for Bioengineering and Nanotechnology (AIBN) unveil a new diagnostic device that could help thousands of lung cancer patients get ahead of the disease before it spreads.
Lung cancer is the most common cause of cancer death in Australia, claiming the lives of nearly 9000 patients each year. Stay on top of our industry news and developments, events and opportunities, by joining The NetworkJoin The Network
PhD scholar Quan says the initial detection and screening can be fairly drawn out and often involves a range of imaging tests and biopsy procedures.
“A patient might first report to their GP when they notice a problem with their chest. They then might get a scan. Then the scan is analysed,” Quan says.
“If there are signs of lesions, you’ve got to see if they’re cancerous or not. And that can involve a lot of very expensive clinical follow ups.”
But a drop of blood is all that is needed for Quan’s surface enhanced Raman scattering microfluidic biosensor to spot the early signs of lung cancer, allowing clinicians to intervene quickly.
“With our technology we can hopefully catch signs of the cancer at that first stage, when there are only very small lung nodules to detect,” Quan says.
Sweet success
In a drop of blood, Quan’s device analyses tiny messenger particles that are known as extracellular vesicles (EVs).
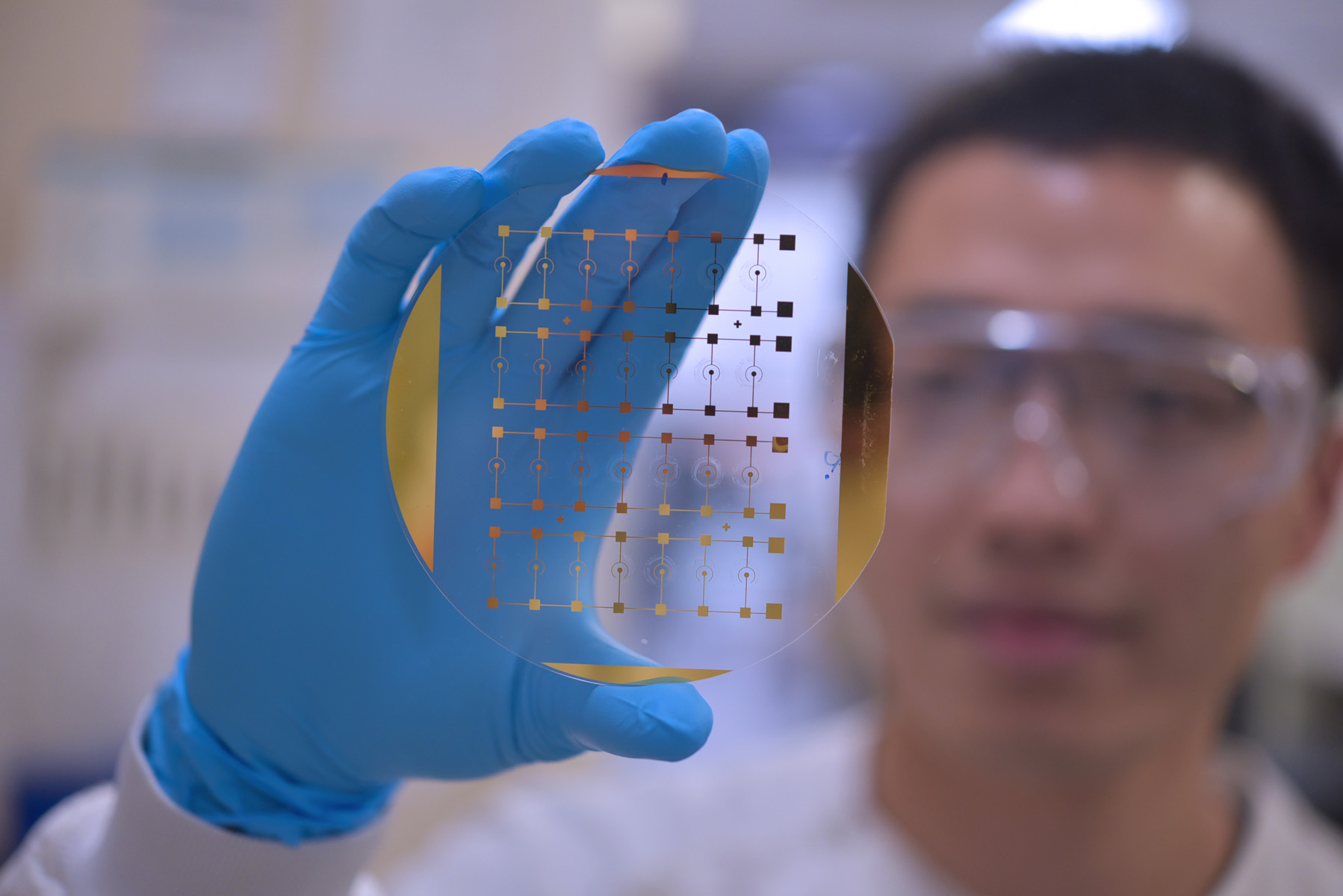
Or, more accurately, it analyses the sugars that coat these EVs.
AIBN research fellow Dr Lobb says the sugars – or glycans – on the surface of EVs serve as an excellent biomarker that can alert clinicians to presence of small lung cancer cells.
“There are a range of different biomarkers you can look for when you’re testing for blood samples for cancer,” says Dr Lobb.
“You could be examining DNA, proteins, even the lipid content. But you’ve also got these extracellular vesicles, and these are coated with sugar molecules of different types.
“And the sugar code is different on a cancer cell compared to a normal cell.
So really, this device is an incredibly non invasive way of picking up when there’s something wrong.
Dr Lobb and Quan are among a number of AIBN researchers who contributed to the Advanced Science paper, including Xueming Niu, Dr Alain Wuethrich, Dr Zhen Zhang, and ARC Laureate and AIBN senior group leader Professor Matt Trau.
In a clinical study evaluated on 40 patients, the team’s technology – a small EV glycan phenotype (EV-GLYPH) assay - successfully differentiated patients with early-stage malignant lung nodules from benign lung nodules.
The results reveal the potential to profile small EV glycans for noninvasive diagnostics and prognostics, opening up promising avenues for clinical applications and understanding the role of small EV glycosylation in lung cancer.
“Ultimately it’s something that could help clinicians step in before more intensive scanning or treatments or drug regimes are needed,” Quan said.
“We’re basically just saying, here’s a blood test. We’ll get the answers we need.”
Also contributing to the Advanced Science paper was Dr Arutha Kulasinghe from UQ’s Frazer Institute, Professor Kenneth O'Byrne from the QUT School of Biomedical Sciences, Associate Professor David Fielding from the RBWH Department of Thoracic Medicine, and Associate Professor Andreas Möller from QIMR Berghofer Medical Research Institute and the Chinese University of Hong Kong.


