The problem, according to Professor Ernst Wolvetang, is that the brain he wants to study is usually still inside someone’s skull.
So that’s why he grows his own.

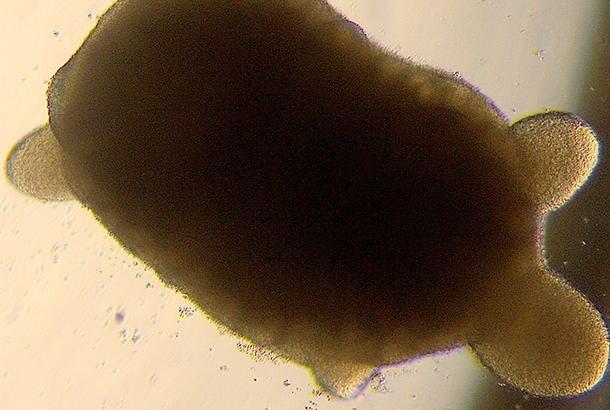
Welcome to the world of organoids: tiny, three-dimensional organ avatars that Ernst and his team are using in the quest for better therapies.
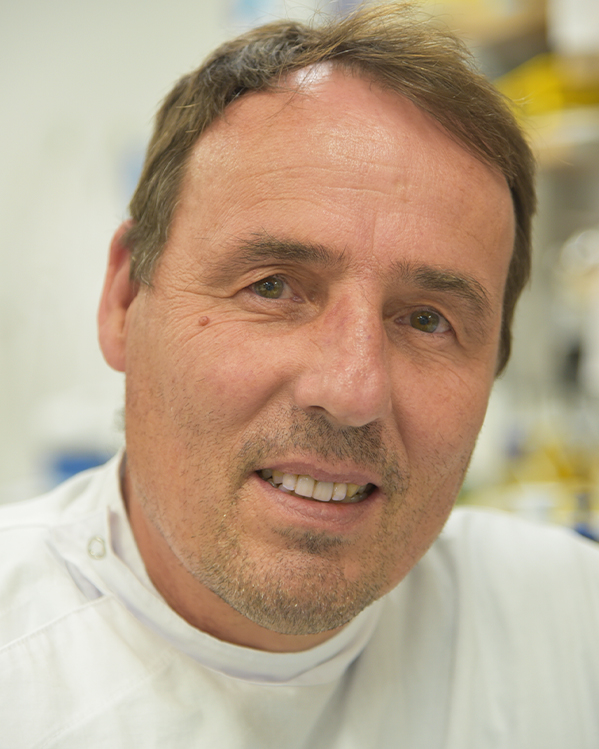
Ernst is one of the more recognisable faces at the Australian Institute for Bioengineering and Nanotechnology (AIBN), and a pioneer in the field of pluripotent stem cell biology.
He was among the first to bring the first human embryonic stem cells to Queensland and his Wolvetang Group is renowned for its work with organoids: growing them, studying them, and using them to try and understand diseases and human development.
“If you want to study someone’s brain at a cellular level, it is very difficult to do it when they are still in in their head,” Ernst says.
“And so we design organoids to recreate that brain – or the person’s heart, or kidneys, or liver – sometimes hundreds of copies that we can study in real time.”
Read on to learn about the story of Professor Ernst Wolvetang, how helping to save the life of a child sent him down the organoid path, as well as the limitless applications he sees on the horizon for artificial organs.
-
Ernst, let’s start from the top. Organoids: what are they?
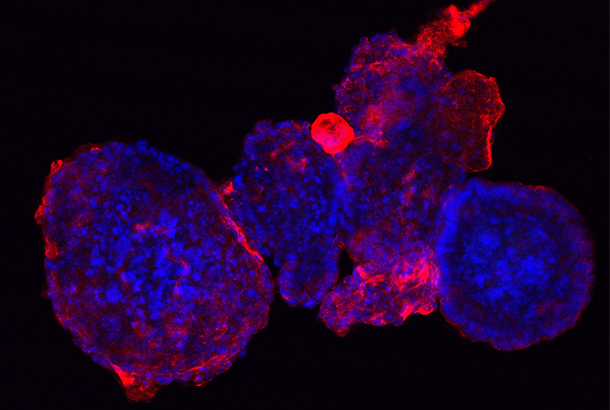
Essentially, we are talking about miniature models of human organs. Brains. Spinal cords. Livers.
We make organoid models using human stem cells that we have created in a dish. We can prompt these cells to develop and grow to have the same structure, architecture and function as the organ they are representing.
They are basically small, three-dimensional avatars.
So tiny organs that act like organs… but aren’t really organs? Why?
Organoids give us a better way to investigate how things go wrong during human development, or how things go wrong during disease. More than that, they allow us to work on therapies to treat diseases.
By artificially making pluripotent stem cells we can capture the uniqueness of an individual. So instead of performing a biopsy on that individual’s brain to study it, you make thousands of organoids that represent the same brain, or specific parts of that brain.
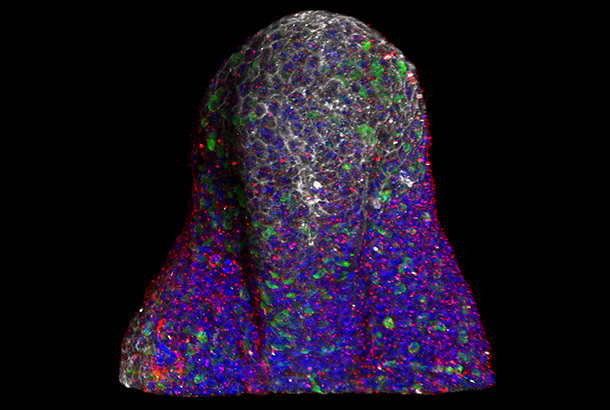
You can make an organoid for the hindbrain - the cerebellum and the spinal cord. You can make hypothalamus where Parkinson's disease sits. You can make the Cortex, where we do our thinking. You can connect those by fusing them.
For all the other organs you can do the same thing. You can make cardiac organoids, liver organoids, kidney organoids. You can make mammary gland organoids that produce human milk.
Primarily now and in the near future, organoids will be used for disease modelling. But we are also seeing a wider scientific purpose.
What else can organoids be used for?
Stay on top of our industry news and developments, events and opportunities, by joining The NetworkJoin The Network
Looking further into the future, transplantation of some organoid types is something that I can see happening. If you are able to grow larger versions of these organoids and have a blood supply… that could make them transplantable, and we could imagine an organoid serving as a functional organ. Dr Hans Clevers in Switzerland and Dr Toshiro Sato in Japan have started to look at organoid transplants for the gut, for problems like stage three bowel disease, where you can make gut organoids and actually put them back into the patients and that will integrate and treat inflammatory bowel disease.
That's where I can see organoids going, as well as other similar arms of regenerative medicine applications.
I also think organoids will be used – especially the brain - as a fundamental tool to understand really enigmatic processes such as consciousness, anesthesia, and fundamental biological processes that are very difficult to study in a wet brain that sits in a real human.
You always rely on imaging inside what you can see from the outside. With organoids we can make so many that we can actually examine the brain in real time and look at the activity of neurons, how they connect, where do things go wrong when it comes to autism, or schizophrenia or epilepsy?
That’s something that you can't do in a real brain so if you can shortcut that it would be a fundamental discovery.
Ernst, can brain organoids … think?
We actually have a PhD student who is really probing this issue. Questions like: ‘where does consciousness come from?’ We can measure correlates, or readouts, of consciousness like gamma waves in our brain organoids. So clearly, they have developed some form of proto consciousness at a particular point in time.
To me, that’s a discovery opportunity to find out exactly what is happening during those couple of weeks? Do the neurons hook up differently with each other? Is it a maturity thing? Can we figure out what drives that? I think that's super exciting. And sort of fundamental to what makes us human right?
Why research things that are small? Right? We research astronomy because we want to find out where our universe comes from and how we were created. And I think this is the same idea. What makes us human? What makes us so unique? Maybe we're not unique? We don't know.
There’s the whole philosophy side of this as well. We published something in the American Journal of Bioethics last year, where we pondered that question. How do you unequivocally determine that something is conscious? And does it then have a moral status? And if it does have a moral status, what is that moral status, because it can be created from a cell of an individual long dead. But the stem cells still exist and you can convince their cells to make thousands of identical organoids that are all showing conscious-like behaviour. So what kind of moral status do they have that right? And how do you find that out? And how do you prove that? And is that ethical?
So that's what I like about human stem cell research. It's edgy. It's at the cutting edge. It can do amazing things, but at the same time, it also butts up against really fundamental things.
Do you think we are far off from seeing organoids embedded in the broader medical industry?
A lot of this stuff is years and years down the track, depending on the organoid model. But some countries have already started to use organoids as a decision-making process as part of their healthcare system.
In Holland, where I'm from, gut organoids are already used to identify the best therapeutics for patients with cystic fibrosis for example. And that is now covered by the pharmaceutical benefits scheme because the government has realised that if you do that you are preserving resources and you get better patient outcomes.
So, you know, in Australia we're a bit behind. I suppose we are trying to bring together the various centres for organoid research nanotechnology and personalised medicine under one group. With that we’ll try and build a clinical interface and show direct patient outcomes.
We've started to do some of that ourselves now with epilepsy already: Making brain organoids from epilepsy patients that are resistant to anti-seizure medications. And the outcomes of screens that we do in the lab are going to be tested for their predictive power in in clinical settings.
Once we have that evidence, and if it is strong, I would hope that health care funders and government will see the value of that, and the value of using this model to pick the right medication for people with epilepsy straight off.
Ernst this is incredible stuff. How did you even come to be working in this field?
I would say my story starts at the Amsterdam Medical Centre – where I did my honours. I was working in a lab that worked on peroxisomal and metabolic disorders.
One day a skin sample came in from a patient, a young boy. It was a baby that had just been born with severe lactic acidosis and was about to die. And so we worked through the weekend to figure out what was wrong. We found a compound that we predicted could rescue him. We tested it on the cells and that was given to the patient immediately, and he survived.
His mum came in a couple of months later with the boy to our lab meeting and said ‘Thank you for saving the life of my boy.’
That's when I went like, okay, this is what I want to do the rest of my life. So I did my PhD in peroxisomal biogenesis disorders.
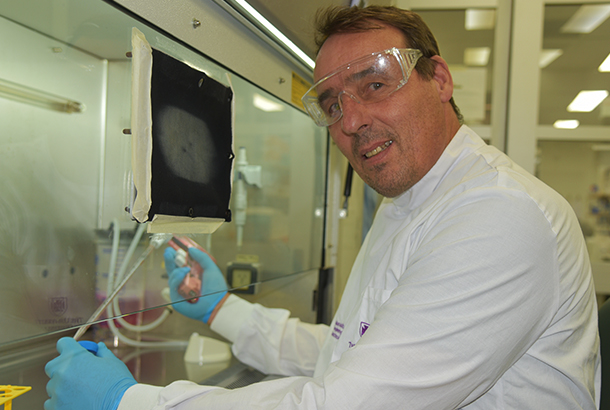
How I got into organoids was when I was in the Centre for Early Human Development at Melbourne and Monash University.
There was a new group leader coming, Martin Pera. He basically brought the first human embryonic stem cells to Australia inside his jacket pocket. I just camped in front of his office and told him “I want to work on human embryonic stem cells”. And basically it started with him inviting me to look at the incubator. He showed me the first cells, told me to figure out how to culture them and how to make different things out of them. And that's how it's done.
Martin then helped to set up the Australian Stem Cell Centre, and later I took over his lab together with another senior postdoc. I came up to UQ and started working with human embryonic stem cells because they were not here in Queensland. So I brought the first ones up here to the AIBN.
In 2009 there was another watershed moment. It was a conference here in Cairns where this guy called Shinya Yamanaka - a Nobel Prize laureate - showed that you can reprogram skin cells back to these same pluripotent stem cells. And I immediately I went to the phone, like the whole rest of the audience, and said “look, forget about embryonic stem cells, we are working on induced pluripotent stem cells from now on”.
So that's when we started to do that at the AIBN and reprogramming cells into pluripotent stem cells to do disease modelling.
Do you think the wider public is truly across the potential of organoid research? Or, at least, do you think they will be?
I think they will be, yes. And especially if the initiatives like uniting the various centres for organoid research can be achieved. As soon as it starts to impact on people's lives and survival – like if we are able to test better anti-cancer therapies - people will start to talk about it.
For example, instead of trying anti-cancer drugs that may or may not work, why not take a biopsy of the cancer, grow several hundred organoids, find the right drug or drug combination that works, and give that to the patient? Once this science becomes mainstream, I think people will flock to hospitals that offer this.
Ernst if we were having this same conversation five years from now, what would you hope to have achieved in your lab?
We'd like to cure two or three diseases.
… any in particular?
Ataxia-Telangiectasia is one. We have a viral therapy for that that we are working on. We're also testing out gene therapies for hereditary spastic paraplegia, and also for white matter diseases that affect kids. 
Those are three flagship projects that are underway at the moment where we use organoid models to test therapeutics. And I suspect they are the ones where we will have the highest chance of having an impact, and maybe even find out why these diseases occur in the first place and if we can do something about it?
If we can I can do that – if we could cure or improve the health outcomes for patients - I could easily hang up my pipet and die a content man.


